Ministers have handed firms £6m in contracts to help devise plans to build a network of new NHS clinics using private capital, despite fears the move could turn into a PFI-style disaster.
The Department of Health and Social Care has awarded contracts worth £3m each to the management consultants Deloitte and the lawyers Addleshaw Goddard. They are advising the DHSC on whether to use public-private partnerships (PPPs) to help build dozens of the promised “neighbourhood health centres” in England.
The firms have been hired to help to develop the business case for pressing ahead with doing so, design what form any PPP could take and draw up the “financial modelling” involved.
In a hint that Labour may decide to join forces with private finance companies on the project, DHSC’s remit to Deloitte and Addleshaw Goddard also includes “potentially supporting [DHSC] through the procurement” of the clinics, which initially will be in deprived parts of the country.
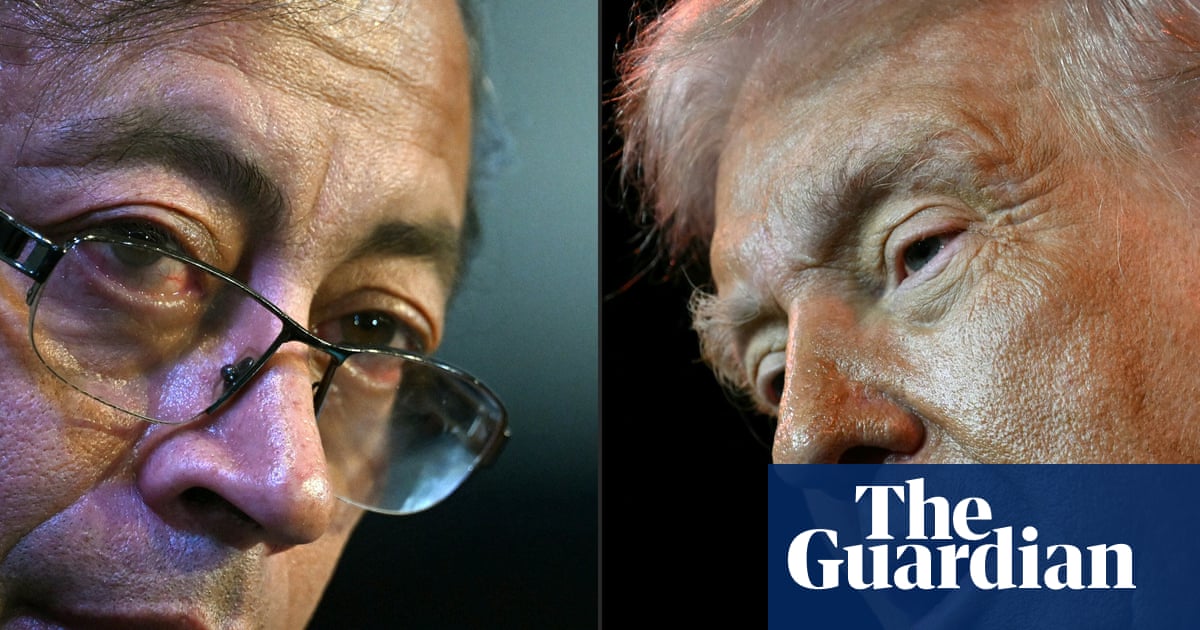
This month Wes Streeting, the health secretary, announced the location of the first 43 centres. Health professionals such as doctors, nurses and pharmacists, social care staff and voluntary groups will provide a range of services under the same roof as part of the government’s plan to move some healthcare from hospitals into community settings.
Campaigners opposed to private sector involvement in the NHS claim that collaborating with it in the rollout of “neighbourhood health centres” risks repeating what the National Audit Office said in 2018 were expensive mistakes made when the private finance initiative (PFI) was used to build scores of hospitals and schools in the 1990s and 2000s.
As a result of those deals the NHS in England is still due to hand private firms more than £40bn until repayments finally end in the 2040s.
“Private finance has been a disaster for our public services,” said Johnbosco Nwogbo, the lead campaigner at the campaign group We Own It. “PFI is a ticking timebomb beneath our NHS, now blowing up in the face of patients.
“Some NHS hospitals are spending more on PFI repayments than on medicines. Profit continues to be taken out by private finance investors, which could be used instead to treat patients.
“While the state of the public finances is dire, the government would be foolhardy and indeed reckless to bring back a version of PFI, given it proved such an expensive rip-off the last time.”
Nwogbo said any Labour tie-up with private capital would break its pledge in its election manifesto that the NHS would “always be publicly owned and publicly funded”.
In response to a freedom of information request from Nwogbo, the DHSC said: “The government is exploring the feasibility of using new public private partnership models for taxpayer-funded projects in very limited circumstances, where they could represent value for money.
“This includes exploring the potential to use PPPs to deliver certain types of primary and community health infrastructure.”
Matthew Taylor, the chief executive of the hospitals group the NHS Confederation, said ministers should consider using the private sector given the NHS’s lack of capital funding to build and repair buildings and buy equipment.
“Given the strain on public finances, private investment is one of the only ways to inject vital capital funding into the NHS so it can build modern healthcare facilities fit for the 21st century,” Taylor said.
“This does not mean resurrecting the old private finance initiatives model, which has faced some justified criticism.” Ministers should learn from how other countries have used PPPs, he added.
A DHSC spokesperson said it was right that it looked at “a range of options to provide the best care for people across the country”.
He added: “All proposals are subject to robust value for money assessments to ensure taxpayers get the best possible return on investment in our health services.”
Rachel Reeves, the chancellor, is due to announce in the budget on 26 November whether private money will be used to help build the clinics.

 3 months ago
64
3 months ago
64