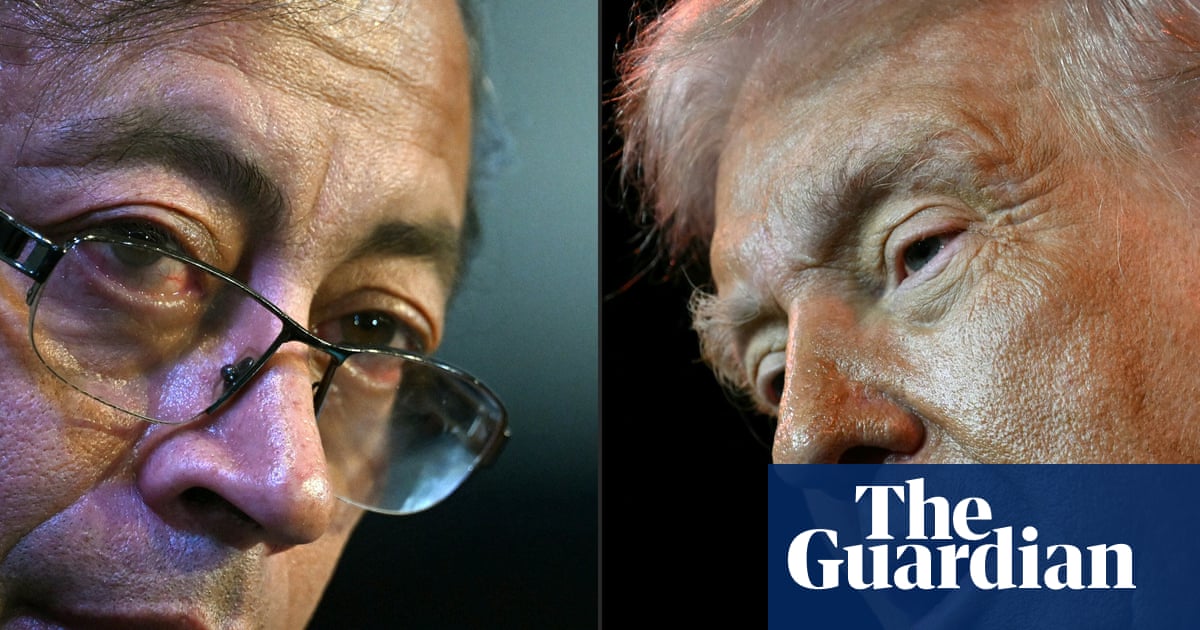
On Monday, Donald Trump, flanked by Robert F Kennedy Jr and the former talkshow host and head of the Centers for Medicare and Medicaid Services, Dr Mehmet Oz, announced that women should avoid paracetamol (known as acetaminophen or by the brand name Tylenol in the US) throughout pregnancy because of a spurious link with childhood autism.
This political theatre highlights a longstanding and harmful problem: pregnant women, and their babies, are routinely let down by partial, poor-quality and missing medical evidence. Pregnant women deserve better than irresponsible headlines raising fear based on shaky research that has failed to convince the scientific community.
Compounding the problem, Trump’s announcement centred women’s choices as the driver of childhood outcomes. Only “if you can’t tough it out” as a pregnant woman, should you resort to treating your own pain and fever, Trump advised. This mistakenly and cruelly pitches women’s needs against the best interests of their baby, rather than seeing a mother and foetus as interdependent. Many women, however sceptical of the Trump administration’s approach to science, will now be burdened with unsubstantiated concerns about how their choices might endanger their pregnancy. Whatever they choose, there is a pathway for them to be blamed.
To be clear: there is no credible evidence linking autism with maternal paracetamol use. The best available research points to the contrary: a large study from 2024 that analysed data from 2.5 million women who gave birth in Sweden, and their babies, found no association between paracetamol use in pregnancy and childhood neurodiversity. The researchers looked at whether mothers of neurodivergent children took paracetamol during pregnancy, but also assessed the presence of known risk factors for autism, the indication for taking paracetamol, and family history of neurodiversity. After accounting for these factors, a childhood autism risk from paracetamol exposure was not identified. No new contradictory evidence was mentioned by Trump that should prompt us to review this reassuring conclusion.
Cases of autism have been rising in recent years, in large part owing to shifting diagnostic categories as well as professional and public awareness about neurodiversity. Risk factors for autism are not fully understood, but include genetic, environmental, pregnancy and social variables. The main factor is your family history: if you are born into a family with siblings and parents who are autistic you are more likely to be too. It is important to underline the stigma that Trump’s announcement will add to neurodiversity diagnoses and the people who live (and thrive) with them.
It is absolutely appropriate to ask the question whether pregnancy exposure to common medicines affects babies in utero and beyond. However, it is dificult to produce definitive answers here; the research is difficult to do well, requiring meticulous design and careful reporting of results. Trump’s announcement was nothing like this; it was essentially speculation, and it could have serious consequences.
Untreated illnesses during pregnancy can be harmful, not only for women’s long-term health, but also for their baby. The “precautionary approach” is often mentioned: if there is any concern about paracetamol, shouldn’t women avoid it to be better safe than sorry? But precaution should go both ways. There is a cost when encouraging pregnant women not to take a effective medicine for pain and fever. These symptoms affect women’s health, functioning and wellbeing, while untreated fever could pose risk to the baby. Research is ongoing, but it appears that maternal fever could have negative effects on the baby’s brain development.
Discouraging paracetamol use risks pushing women who are in need of pain relief towards unlicensed treatments or alternative analgesia such as ibuprofen. Unlike paracetamol, ibuprofen poses proven risks in pregnancy in different trimesters, including miscarriage, foetal kidney damage and premature closure of an important blood vessel (the ductus arteriosus) in the foetus. These risks far outweigh any possible link between paracetamol and childhood autism.
Today is an opportunity to discuss how we assess the safety of medicines in pregnancy. Few research studies include equal numbers of women and men, and the data is often not compared appropriately to see if there are sex differences in outcomes. Even fewer medicines are studied in pregnancy. After the thalidomide and sodium valproate scandals, there are still understandable public fears about the potential harm of medication on babies, although neither of these drugs were studied in pregnant women before reaching the market. Rather than exporting risk at scale into the population, efforts should be made to build the evidence base safely by bringing pregnant women who want to be involved into biomedical research.
That’s why Dr Ed Mullins, an obstetrician, and I are collaborating on Message Maternity, a project to bring together healthcare researchers, research funders, medicines regulators, legal experts and medical publishers and most importantly women themselves to understand why those who are pregnant are routinely excluded from research, and how we might safely and respectfully change the culture from exclusion towards inviting women’s inclusion in support of patient autonomy, and informed decision making. We want to minimise harm on an immense scale, which could occur when pregnant women are given incorrect medical advice.
after newsletter promotion
Covid-19 vaccine exclusions highlighted what many researchers and women had felt for a long time: medical research should be moving towards greater inclusion of pregnancy in studies. What women need is high-quality scientific evidence, based on robust data that considers risks and benefits that can then be considered against their personal situation. This overreaching, politically motivated announcement in the US will only push that cause backwards.
-
Kate Womersley is a doctor and academic specialising in psychiatry

 3 months ago
70
3 months ago
70